Digestive System and abdomen
Learning Objectives:
- Identify the major organs and accessory organs of the digestive system
- Describe the functions of the enzymes involved in digestion of food
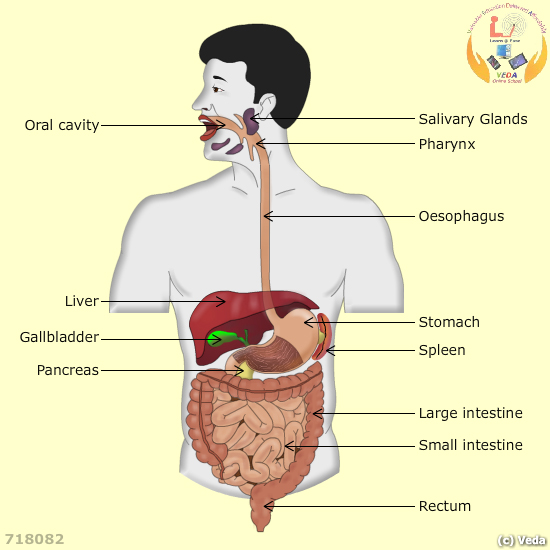
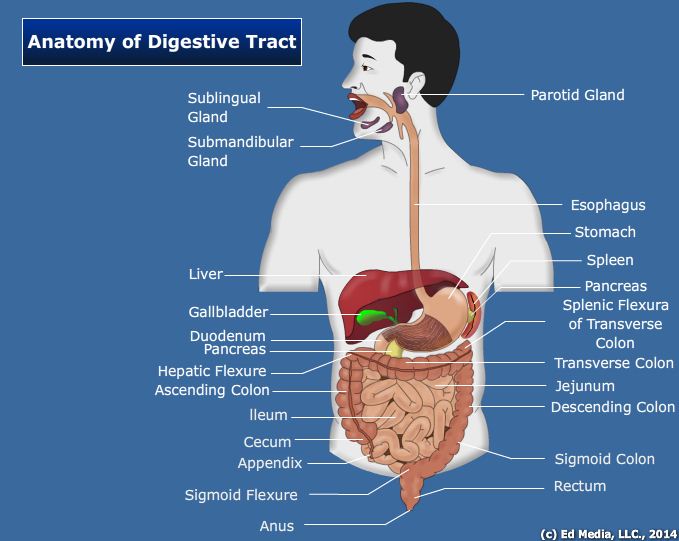
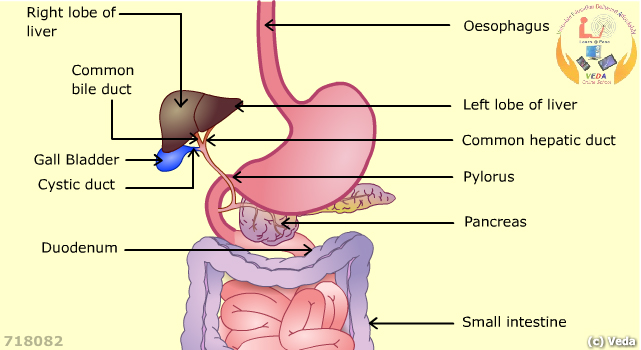
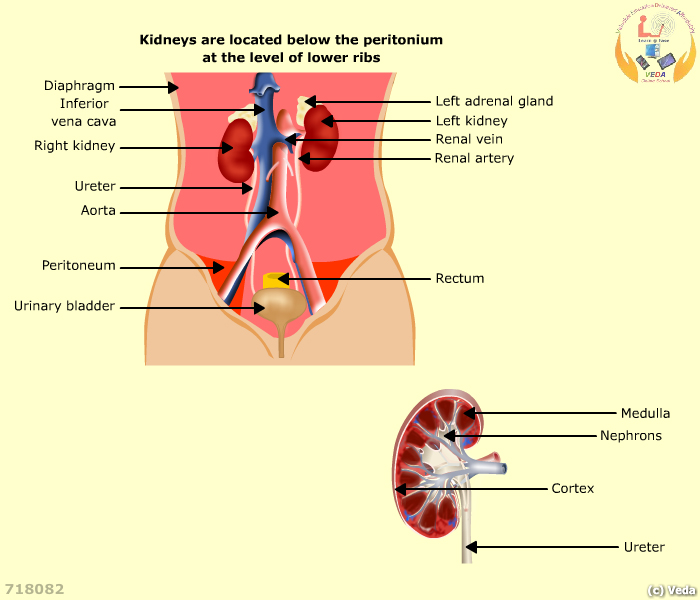
IntroductionThe digestive system consists of the major organs and accessory organs that convert complex organic molecules into a simpler form that can be absorbed. It includes a series of organs forming a hollow tube called the gastrointestinal tract. It extends from the mouth to the anus. The path of the gastrointestinal tract starts with mouth followed by pharynx, esophagus, stomach, small intestine, large intestine, rectum, and the anus. The space formed in the gastrointestinal tube is called the lumen and helps to pass food and liquid. The whole of the gastrointestinal tract has certain structural characteristics in common.
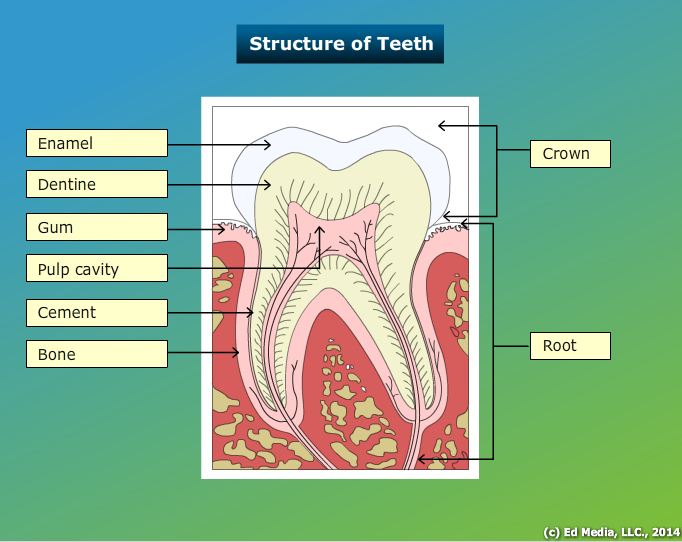
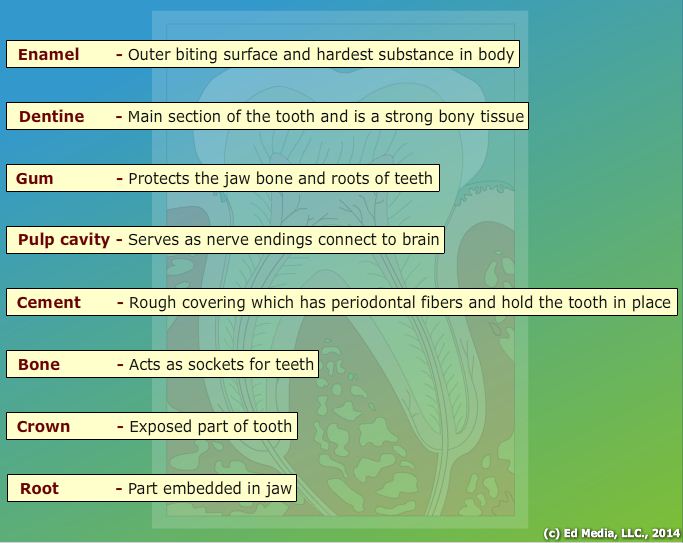
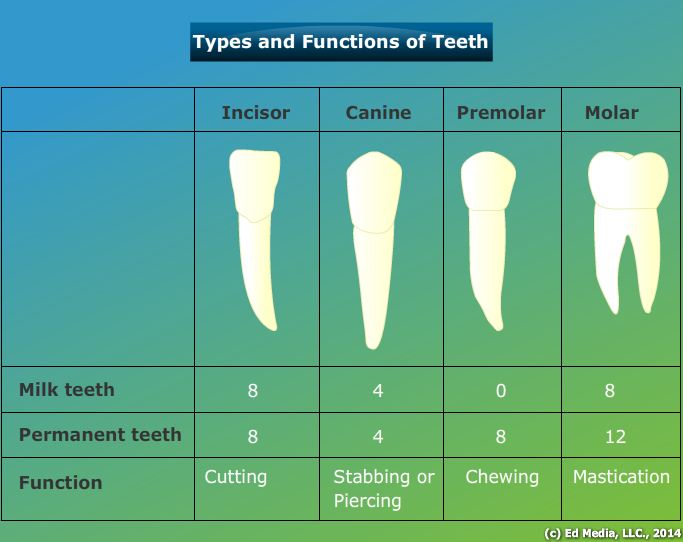
Generally, the alimentary canal starts with mouth, which contains different types of teeth. The following animation will discuss the structure, types, and function of teeth.
Proper digestion of food depends on the enzymatic functions of the various secretions found throughout the digestive system. These secretions help digest the macromolecules of food by breaking them into smaller molecules and facilitating their absorption. Various organs located in digestive tract secrete digestive enzymes including the mouth, stomach, pancreatic, and intestinal cells. The accessory organs consist of the salivary glands, gallbladder, liver, and pancreas.
The digestive enzymes target different substrates. Digestive enzymes are classified based on their target substrates:
- Proteases and peptidases split proteins into their monomers, amino acids.
- Lipases split fat into three fatty acids and a glycerol molecule.
- Amylases split carbohydrates such as starch into simple sugars.
- Nucleases split nucleic acids into nucleotides.
The following media explains about the Digestion in Humans:
The following media explains about the Physiology of Digestion:
Oral CavityMajor Salivary GlandsThree pairs of major salivary glands and some minor salivary glands secrete saliva in the human body. They occur in pharyngeal mucous membrane. Some important salivary glands are the parotid, submaxillary (or submandibular), and sublingual glands.
- Parotid Glands: the largest salivary glands present. These glands are located in the face just below and in front of the ear. Each gland weighs between 20 to 30 grams. The oral cavity receives saliva secretions from these glands. A duct named Stensen’s duct passes saliva to the oral cavity. This duct opens at the side of the upper second molar tooth.
- Submaxillary Glands: also known as the submandibular glands. These glands occur in the submaxillary triangle medial to the mandible. The weight of the gland varies from 8 to 10 grams. Saliva from these glands empties into the oral cavity through Wharton’s duct. This duct opens at the side of frenulum of tongue by a small opening on the summit of papilla called caruncula sublingualis.
- Sublingual Glands: the smallest of the major salivary glands. These glands are located in the floor of the mouth. Each gland weighs between 2 and 3 grams. There are small ducts called the ducts of Rivinus that obtain salivary secretions from the sublingual glands and provide saliva to the underside of the tongue.
Minor Salivary Glands
- Lingual mucous glands: present on the posterior side of the tongue behind the circum vallate papillae.
- Lingual serous glands: present in the submandibular gland, and to a lesser extent, on the sublingual gland. These glands secrete enzymes such as alpha-amylase.
- Buccal glands: situated between the mucous membrane and the buccinatory muscle. Four of five of these glands are also present outside of the buccinators around the parotid ducts.
SalivaComposition: Saliva is composed of 95.5% water and 0.5% solids, which include enzymes and other organic substances. These components include amylase, lingual lipase, lysozyme, lactoferrin, secreted IgA, phosphatases, carbonic anhydrase, and kallikrein. Organic substances present in saliva include proteins, blood group antigens, free amino acids, nonprotein nitrogenous substances such as urea, uric acid, creatinine, xanthine, and hypoxanthine. Inorganic substances present include sodium, calcium, potassium, bicarbonate, bromine, chloride, fluoride, and phosphate.
Functions: Saliva performs several vital functions in the digestive system:1. Preparation of food for swallowing.Saliva moistens food and enables easier chewing and swallowing. The moistened and masticated food is rolled into a bolus, which is lubricated by the mucin of saliva.
2. Appreciation of tasteAs the solid food is broken down by salivary action, the dissolved substances stimulate the taste buds, enabling the sensation of taste.
3. Digestive functionSaliva aids digestion via three digestive enzymes, which are salivary amylase, maltase, and lingual lipase. Salivary amylase and maltase digest carbohydrates while the lipase digests fat.
4. Cleaning and protective functionConstant secretion of saliva ensures that the mouth and teeth are rinsed and kept free of food debris. Epithelial cells and foreign particles are removed due to salivary secretions. Saliva prevents bacterial growth in the mouth: an enzyme called lysozyme kills bacteria of the genera Staphylococcus, Streptococcus, and Brucella present in the mouth.
5. Role in speechThe lubrication provided by saliva moistens the mouth and aids speech by enabling better pronunciation.
6. Excretory functionSubstances such as mercury, potassium, iodide, lead, and thiocyanate are removed by saliva in the body. Salivary secretions also remove viruses that cause rabies and mumps. During nephritis, excessive urea gets excreted in saliva. When hyperparathyroidism occurs excess calcium also is removed through the saliva.
7. Regulation of water balanceDuring periods of dehydration, the body minimizes salivary secretions, which induces the feeling of thirst. The following media explains about the Functions of Saliva:
The following media explains about the Positions of Taste Buds:
Function of salivary glandsSalivary glands in the mouth secrete an array of substances.
- Potassium bicarbonate (
): Neutralizes acid and enhances preservation of dentin and tooth enamel. It also balances bacterial toxins. Bicarbonate prevents acid damage this is caused in esophageal lining before food enters the stomach.
- Lingual lipase: With the help of this enzyme lipid digestion begins in the mouth.
- Amylase: Enzyme produced by the salivary glands that breaks down complex carbohydrates to smaller links or even simple sugars. The other name of the amylase is ptyalin.
- Mucin: Functions mainly to make food more pliable by lubricating the content.
- Lysozyme: the bacteria and viruses in food are killed by lysozyme. Lysozyme therefore serves beneficial anti-septic function in digestion.
- IgA: A sort of dimeric form of antibodies produced by the body. Gastrointestinal tract makes IgA mainly to battle bacterial toxins and virus.
- Haptocorrin: also known as R-factor. Haptocorrin has an important function: protecting vitamin B12.
The following media explains about the Mouth and Buccal Cavity:
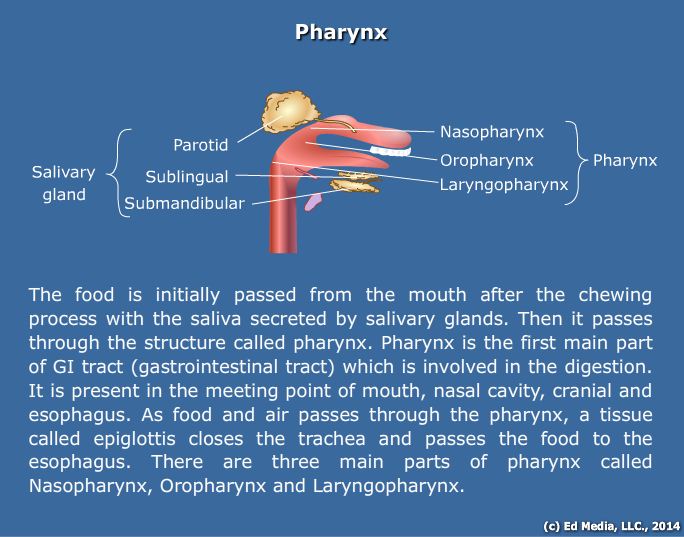
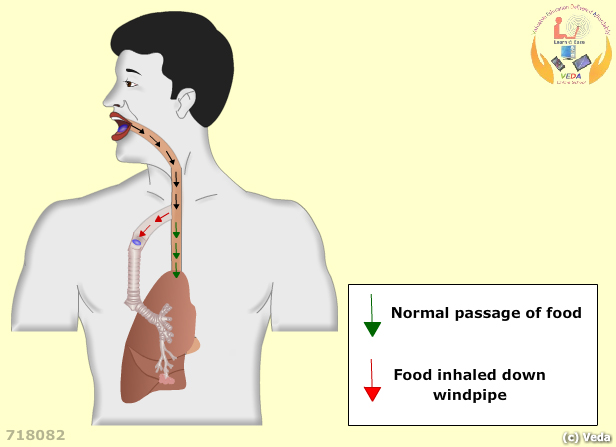
PharynxThe pharynx extends from the mouth and back of the nasal cavity to the esophagus. This cavity is also connected to the larynx. Composed of the nasopharynx, oropharynx, and the laryngopharynx, the pharynx serves an important role in the ingestion of food by connecting the oral cavity with the larynx and esophagus. The epiglottis is a flaplike structure in the larynx that closes off the trachea so that that food does not enter the respiratory tract.
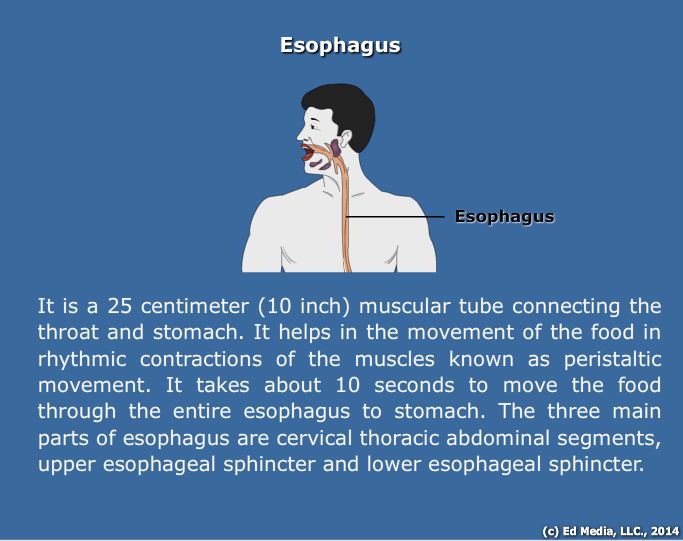
Esophagus The esophagus, which connects the pharynx and the stomach, is a muscular tube that is made of both skeletal and smooth muscle, and is therefore under both somatic and autonomic nervous control. Peristalsis refers to the rhythmic contraction occurring in the muscle that allows food to travel toward the stomach.
The upper esophageal sphincter allows food that is swallowed to travel to the top of the esophagus. The lower esophageal sphincter (cardiac sphincter) is found near the bottom of the esophagus and relaxes to allow food to enter the stomach.
The following media explains about the Food Pipe:
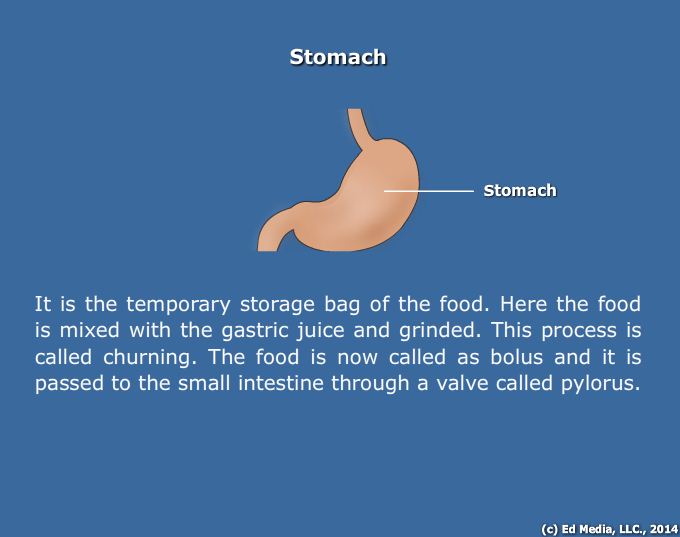
Stomach The stomach plays a major role in both mechanical and enzymatic digestion. It is a muscular organ that is characterized by its highly acidic environment that facilitates the breakdown of food particles. It receives food from the esophagus, mixes it with various secretions, and moves the food to the small intestine. The stomach is divided into the cardiac, fundic, body and pyloric regions. The pyloric sphincter controls gastric emptying into the small intestine. The following secretions in the stomach play key roles in digestion:
- Pepsinogen: the main gastric enzyme produced by stomach cells. Chief cells secrete pepsinogen, which is the inactive zymogen form of pepsin. Pepsinogen is cleaved to pepsin in the presence of HCl. Pepsindigests proteins found in food into smaller particles, such as peptide fragments and amino acids. Protein digestion therefore begins in the stomach.
- Hydrochloric acid (HCl): HCl functions to denature the proteins ingested, to destroy any bacteria or viruses that remain in the food, and to activate pepsinogen into pepsin.
- Intrinsic factor (IF): Intrinsic factor is a glycoprotein produced by the parietal cells of the stomach. Its main function is to enable the proper absorption of vitamin B12.
- Mucin: The stomach must be able to destroy bacteria and viruses using its highly acidic environment while also protecting its own lining from the acid. Mucin and bicarbonate serve to protect the stomach cells from the effects of an acidic environment.
- Gastrin: This is an important peptide hormone produced by the “G cells” found in the pyloric glands of the stomach. G cells produce gastrin in response to stomach stretching occurring after food enters it, and also after stomach exposure to protein. Gastrin is an endocrine hormone and therefore enters the circulation of blood and eventually returns to the stomach where it stimulates parietal cells to produce their hydrochloric acid (HCl) and Intrinsic factor (IF). Gastrin stimulates the stomach to contract in order to mix its contents into an acidic mixture called chyme.
The following media explains about the Stomach:
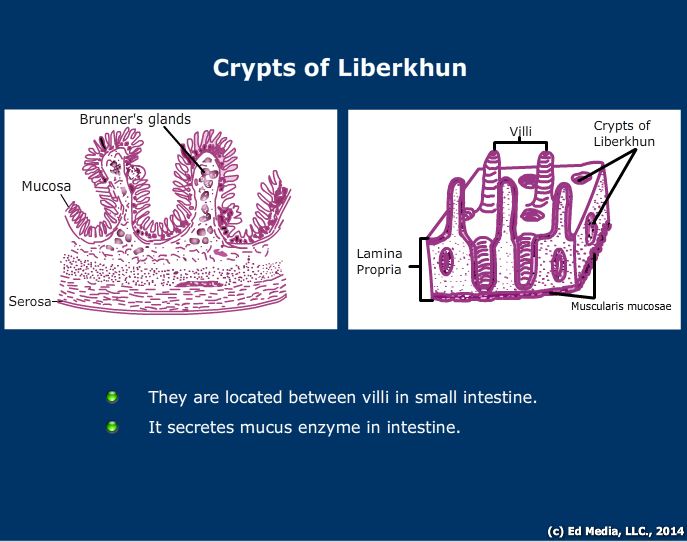
DuodenumThe duodenum is one of three segments found in the small intestine. While the other two segments, the ileum and the jejunum, are responsible for absorption, the duodenum is responsible for chemical digestion.
When chyme leaves the stomach via the pyloric sphincter, it enters the duodenum for further chemical digestion. The key secretions that take part in the digestive process in the duodenum are:
- Brush border enzymes: release of chyme into the duodenum stimulates the release of brush border enzymes, which are found in the cells lining the duodenum. These enzymes include maltase, isomaltase, lactase, and sucrase, which break down disaccharides, maltose, isomaltose, lactose, and sucrose, respectively.
- Peptidases: break down proteins or peptides.
- Enteropeptidase: an enzyme that activates trypsinogen to trypsin and procarboxypeptidases A and B to their respective active forms.
- Secretin: This is an endocrine hormone produced by the duodenal “S cells” in response to the acidity of the gastric chyme. It acts to regulate pH in the digestive tract by increasing bicarbonate secretion from the pancreas in order to counteract HCl secretion from parietal cells.
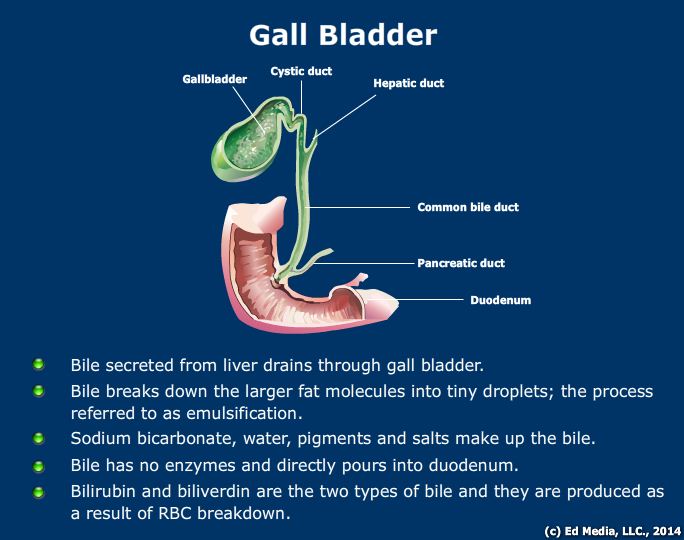
- Cholecystokinin (CCK): CCK is a peptide hormone that functions to stimulate the release of pancreatic juices and bile. Bile is a fluid comprised of cholesterol, bile salts, and pigments. Bile salts, which are derived from cholesterol, serve to emulsify fats and cholesterol into micelles.
- Somatostatin is a hormone produced by the mucosal cells of the duodenum and also the “delta cells” of the pancreas. Somatostatin has a major inhibitory effect on pancreatic juice production.
- Gastric inhibitory peptide (GIP): This peptide decreases gastric motility and is produced by duodenal mucosal cells.
- Motilin: this substance increases gastro-intestinal motility via specialized receptors called “motilin receptors.”
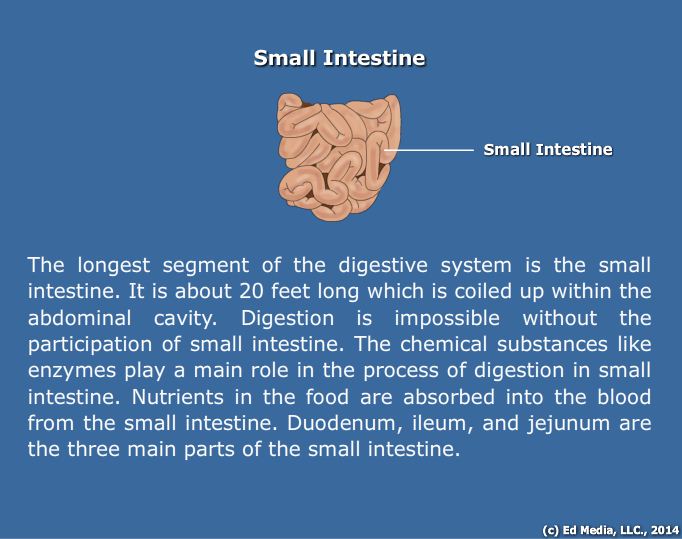
The following media explains about the Small Intestine:
The following media explains about the Absorption of Small Intestine:
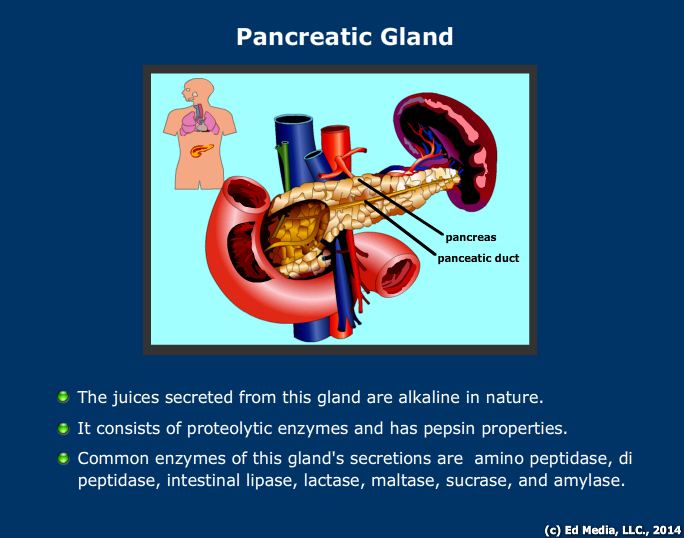
Pancreas The pancreas is both an endocrine and an exocrine gland. As an endocrine gland, it releases hormones such as insulin and glucagon, which are necessary to maintain blood glucose levels and regulate glucose metabolism, in the body, into the bloodstream. As an exocrine gland, the pancreas produces digestive pancreatic juice via acinar cells. Pancreatic juice is secreted eventually via the pancreatic duct into duodenum. This digestive juice functions to break down all three classes of biomolecules (proteins, carbohydrates, and fats). It is made up of the following enzymes:
- Pancreatic amylase: breaks down larger polysaccharides into smaller subunits, and is mainly responsible for the digestion of carbohydrates.
- Pancreatic peptidases: include trypsinogen, chymotrypsinogen, and carboxypeptidases A and B. These are released initially in their zymogen forms and are activated by enteropeptidase that is produced by the duodenum. Once activated, these peptidases are responsible for digesting proteins.
- Pancreatic lipase: functions to breakdown fats into glycerol and fatty acids.
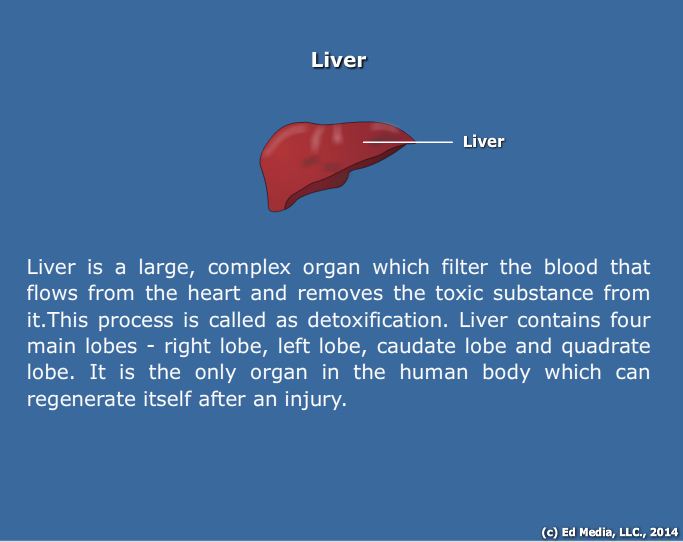
Liver The liver produces bile that is important to digestion. Bile functions to break down fat globules into smaller droplets called emulsification. Enzymes can digest the fat droplets more efficiently due to the larger surface area. Bile is produced in the liver, stored in the gall bladder and transported to the small intestine through bile ducts.
Bile is comprised of cholesterol, bile salts, and pigments. Bilirubin is the main pigment found in bile and is a byproduct of the breakdown of hemoglobin. The daily amount of bilirubin resulting from the destruction of red blood cells is around 250~300 mg. Bilirubin splits to heme and globin at first, then is further split to iron and biliverdin, before biliverdin is finally converted to bilirubin. Bilirubin combines with albumin in the blood stream and is separated into liver cells. Bilirubin in the hepatocytes conjugates with glucuronic acid to become conjugated bilirubin, which is excreted from hepatocytes to the biliary tract and intestines and finally excreted out of the body. The original bilirubin from hemoglobin is free unconjugated bilirubin in the blood stream, and is not soluble in water. After being taken into hepatocytes, it is converted to soluble conjugated form, which can then be excreted into bile ducts.
The liver serves many such biochemical functions, including the following:
- Produces bile, which helps lipid digestion.
- Converts glucose to glycogen and helps control blood sugar levels.
- Acts as a storehouse for biomolecules such as carbohydrates, proteins, lipids, iron, copper, and vitamins A, D, E, and K.
- Helps regulate fluid balance in the blood.
- Is involved in red blood cell formation in the embryo and in some abnormal states, forms blood in adults.
- Removes foreign bodies by phagocytosis using Kupffer cells.
- Forms an anticoagulant called heparin.
The following media explains about the Functions of Liver:
The following media explains about the Formation of Prothrombin in Liver:
The following media explains about the Bilirubin Metabolism:
Most common signs and symptoms of gastrointestinal disorders:
- Gastrointestinal (GI) symptoms such as
- Heartburn,
- Indigestion/dyspepsia,
- Bloating and constipation are common in the community.
Digestive System Diseases:
- Crohn disease. Crohn disease, chronic inflammation of the digestive tract, usually occurring in the terminal portion of the ileum, the region of the small intestine farthest from the stomach.
- Celiac disease
- Cholera
- Jaundice
- Gastroenteritis
- Gastroesophageal re flux disease
- Dysentery
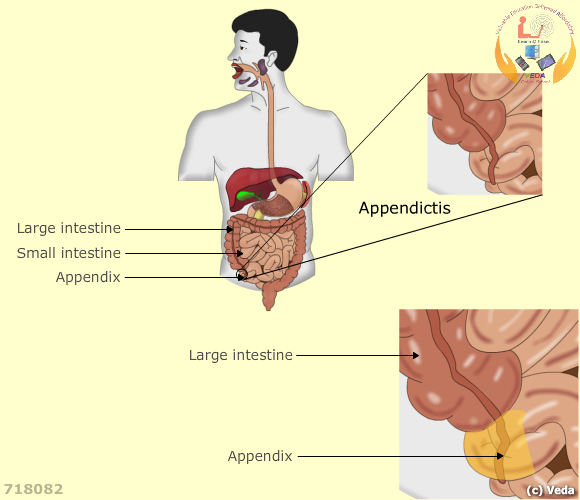
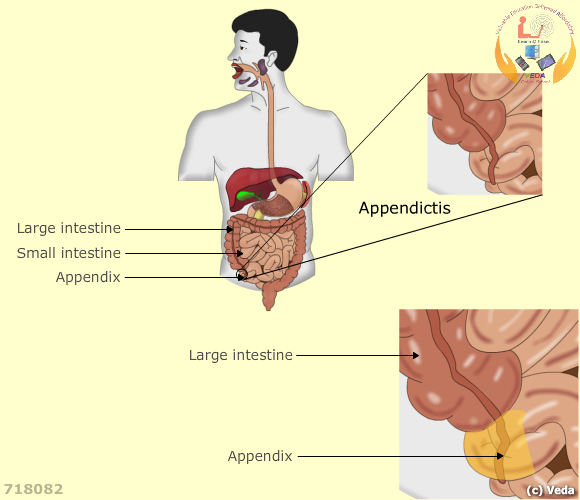
- Appendicitis
Appendicitis:
Points to remember:
Appendicitis is an inflammation of the appendix, a finger-shaped pouch that projects from your colon on the lower right side of your abdomen. Appendicitis causes pain in your lower right abdomen.
The classic symptoms of appendicitis include:
- Dull pain near the navel or the upper abdomen that becomes sharp as it moves to the lower right abdomen
- Loss of appetite
- Nausea and/or vomiting soon after abdominal pain begins
- Abdominal swelling
- Fever of 99-102 degrees Fahrenheit
- Inability to pass gas