Learning Objective:
- Understand the primary function of the circulatory system and its physiology.
- Trace the flow of blood through the heart
- Describe the structure of the heart.
- Describe the conducting system of the heart
- Compare/contrast the structure and function of arteries, capillaries and veins.
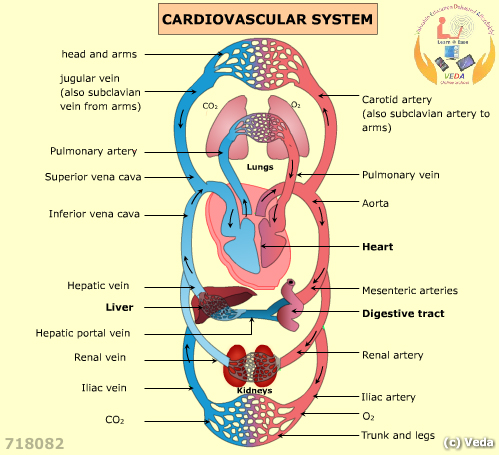
IntroductionThe cardiovascular system consists of the blood, heart and blood vessels and functions in the exchange of nutrients and chemicals between the external environment and body cells. Humans have a closed circulatory system that means that the blood is confined to blood vessels. This configuration allows for a higher blood pressure so blood can move by bulk flow through the arteries. Capillaries are the site of exchange (by diffusion, filtration and osmosis) for materials between the blood and the interstitial fluid surrounding the cells.
The circulatory system is responsible for the transportation of water, nutrients, oxygen, hormones, and waste materials such as carbon dioxide and urea throughout the body. The circulatory system plays a major role in cell metabolism by transporting nutrients from the intestine, oxygen from the lungs to the entire body and by eliminating carbon dioxide from the body.
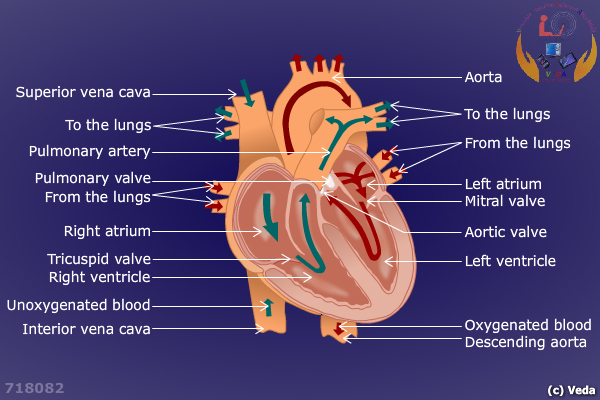
Physiology of circulationThe human heart is four chambered and is considered a double pump. The cardiovascular system is comprised of the pulmonary, systemic and coronary circulations. The pulmonary circuit consists deoxygenated blood traveling to the lungs from the right ventricle and returning to the left atrium. The systemic circulation consists of the oxygenated blood traveling from the left ventricle to the rest of the body and returning to the right atrium. Coronary circulation refers to the movement of blood in the blood vessels of the heart. Two types of valves, semilunar (SL) and atrioventricular (AV), allow blood to flow only in one particular direction.
The following media (Heart) explains about the Heart:
Passage of blood through the heart:
- Oxygen-depleted blood enters the right atrium through the superior and inferior vena cava. The superior vena cava returns blood from parts of the body located above the heart, and the inferior vena cava returns blood from parts of the body located below the heart.
- Deoxygenated blood enters the right atrium, moves through the tricuspid valve, and enters the right ventricle.
- When contraction occurs, blood in the right ventricle passes through the pulmonary valve and enters the pulmonary arteries. The arteries continue in smaller and smaller vessels until they reach the lungs.
- Blood reaches the capillaries lining the alveoli, participating in gas exchange by trading carbon dioxide for oxygen.
- The newly oxygenated blood then goes into pulmonary venules, then into pulmonary veins, which then transport the blood to the left side of the heart. It then travels into the left atrium, through the mitral valve, and into the left ventricle.
- When contraction occurs, blood in the left ventricle passes through the aortic valve and into the aorta. Blood then travels to arteries, arterioles, and then capillaries.
- The oxygenated blood participates in gas exchange at the capillaries.
- Deoxygenated blood enters the venules, and into the larger veins. Eventually, the deoxygenated blood enters the superior vena cava or the inferior vena cava to enter the right side of the heart.
The following media (Cardiac Cycle) explains about the Cardiac Cycle:
In humans, the heart contracts (systole) and relaxes (diastole) about 70 times a minute. Each heartbeat lasts about 0.85 seconds. A familiar lubb-dupp sounds occurs when the valves close. Vibrations occurring when ventricles contract leading to atrioventricular valve closure cause the lower long-pitched “lubb”. The shorter and sharper “dupp” occurs when semilunar valves close when the ventricles relaxes. A heart murmur or a slight swishing sound after lubb occurs which is due to leaky valves, which allow blood to pass back into the atria after the atrioventricular valves have closed.
Since the left ventricle requires greater pressure to pump, its walls are thicker than the right ventricle (which pumps blood across a shorter distance). Thus, blood pressure is greatest in the aorta. It then decreases as the total cross-sectional area of arteries and then arterioles increases.
Intrinsic control of heartbeat
The intrinsic control of heartbeat leads to rhythmic contraction of the atria and the ventricles. The two types of nodes found in the human heart are the sinoatrial node (SA node) and the atrioventricular node (AV node). The SA node is positioned in the upper dorsal wall of the right atrium and the AV node is found at the base of the right atrium, near the septum. The SA node is termed as the pacemaker of the heart as it helps to maintain regular heartbeat by generating an impulse.
The heartbeat is initiated by the excitation impulse passed on from the SA node every 0.85 seconds. This excitation impulse causes the atria to contract. Slight delays are observed when the impulse reaches the AV node that allows the atria to finish their contraction before the ventricles begin their contraction. Ventricles contract after receiving impulse from the AV node through two branches of atrioventricular bundle (AV bundle) before reaching the numerous and smaller Purkinje fibers. The AV bundle, its branches, and the Purkinje fibers are comprised of specialized cardiac muscle fibers that efficiently cause the ventricles to contract.
The following media (Conducting System of the Heart) explains about the Conducting System Of The Heart:
Extrinsic control of heartbeat
The body has an extrinsic way in regulating the heartbeat. Cardiac control center is present in the medulla oblongata, a portion of the brain that helps control the internal organs. The heartbeat is controlled by the autonomic nervous system, which is divided into the sympathetic and parasympathetic nervous systems. Signals from the sympathetic nervous system speed up the heart rate and increase contractility of cardiac muscle. Parasympathetic signals slow down the heart via decreases in SA and AV nodal activity.
Blood Vessels
Learning objective:
- Identify the different types of blood vessels and their unique functions.
- Be able to understand the physiological similarities and differences among the different vessels
ArteriesThe artery has three layers or tunics. The innermost layer of an artery (tunica interna) is made up of simple squamous epithelial cells called endothelium. A thick layer of smooth muscle fibers and elastic connective tissue makes up the middle layer (tunica media) of an artery. The outer layer (tunica externa) is relatively thin and is made up of connective tissue and elastic fibers.
Arteries transport blood away from the heart to the lungs and other organs in the body. The support to an artery under pressure is provided by the strong architectural walls, which are muscular and elastic in nature. When pressure is created in the blood vessels the elastic tissue helps them to expand in order to absorb the pressure.
Arteries branch into arterioles, which hold similar structural features as that of the artery. The middle layer is composed of smooth muscle and is elastic in nature. The vessel constricts when these muscle fibers contract. On the contrary, when the vessel dilates, these muscles relax. Constriction and dilation of arterioles have a direct effect on blood pressure. The greater the number of vessels dilated, the lower the blood pressure.
Capillaries
Arterioles branch into capillaries, which are extremely narrow, microscopic structures. Capillaries are composed of one-cell thick walls made up of endothelium along with a basement membrane. The thin walls of the capillary mean that gases, nutrients, hormones, and wastes can easily diffuse through. Capillary beds are present in all regions of the body. In the tissues, only certain capillary networks are open at any given time. Since capillaries are delicate, damages to them can cause blood to leak into the interstitial space, giving rise to bruises.
VeinsVeins are thin vessels that return blood from the body to the heart. They have larger lumens and thinner tunica media than arteries. Blood in the capillaries is drained by the venules, which are smaller venous structures that rejoin to form veins. Walls of the veins are similar to the arteries in that they contain three layers. However, veins contain less smooth muscle and less elastic tissue than arteries. The thinner walls of veins give them far less elasticity than arteries.
The blood flow is restricted towards one direction due to the presence of valves that help prevent backflow when closed. Additionally, veins rely on external forces to push blood up to the heart against gravity. Skeletal muscles surrounding the veins aid by contracting and squeezing them, forcing blood in an upward direction. Veins also function as a reservoir for blood.
The following media (Blood Vessel) explains about the Blood Vessel:
The following media (Veins and Capillaries) explains about the Veins and Capillaries:
Blood pressure
Learning Objectives:
- Understand the importance of maintaining blood pressure at a proper level.
- Learn the mechanisms through which the body maintains a sufficiently high blood pressure.
Blood pressure is the pressure exerted by blood against the wall of a blood vessel. A sphygmomanometer is used to measure blood pressure. Blood surges to the arteries causing the elastic walls to stretch but then immediately recoil. This rhythmic expansion and recoil of an arterial wall can be felt as pulse in artery running close to the body’s surface. Normally the pulse rate indicates the rate of heartbeat because the arterial walls pulse when the left ventricle contracts. The pulse rate is usually 70 beats and can vary from 60 to 80 per minute among individuals. Normal resting blood pressure, expressed as a ratio of the systolic and diastolic pressures, for a young adult is 120 mm Hg over 80 mm Hg, and can be represented as 120/80. Blood pressures vary throughout the body and are highest in the aorta and lowest in the vena cava.
Blood pressure must be adequately high so that blood may be pumped forward, so information regarding blood pressure is important to assess the effectiveness and function of the circulatory system.
Baroreceptors, which are neurons that sense pressure changes, regulate blood pressure in the walls of the vasculature by responding to changes in arterial wall tension. When blood pressure is low, baroreceptors trigger vasoconstriction by stimulating the sympathetic nervous system.
Chemoreceptors are also involved in the regulation of blood pressure. During times of dehydration when the osmolarity of blood is high, ADH (antidiuretic hormone) is released, causing the reabsorption of water. This causes an increase in blood volume, and therefore, blood pressure.
Cardiac Cycle and the ECG
Learning Objectives:
- Understand the purpose and function of an ECG.
- Identify the PQRS waves and what they represent.
Regulation and Detection of Cardiac Activity
DefinitionThe Electrocardiogram (ECG) machine is a medical device that records the electrical activity of the heart. It is externally recorded using the skin electrodes. Excitation spreading through the myocardium produces local electrical potential. It causes small currents to flow through the body. A suitable electrode can collect these currents in the form of electrocardiogram.
Clinical useECG is useful in determining and diagnosing the following:
- Abnormal rhythms of the heart.
- Heart rate, arrhythmias, abnormal electrical conduction
- Poor blood flow to heart muscle and damage to the conductive tissues
- Heart attack, coronary artery disease.
- Hypertrophy of the heart chambers.
ECG Leads system
Bipolar leadsLeads are connected to the electrocardiograph, each compromising two or more electrodes that are attached to specific site of the body and examine to electrical activity by monitoring changes in the electrical potential. Lead I the standard bipolar limb lead attached to the right and left arms.Lead II the standard bipolar limb lead attached to the right arm and left leg.Lead III the standard bipolar limb lead attached to the left arm and left leg.
Unipolar leadsUnipolar leads which connected to theV1: right 4th intercostal spaceV2: left 4th intercostal spaceV3: halfway between V2 and V4V4: left 5th intercostal space, mid-clavicular lineV5: horizontal to V4, anterior axillary lineV6: horizontal to V5, mid-axillary line
The PQRS wavesRegular wave patterns can be observed in the ECG recordings of a normal patient. It consists of a P wave, a QRS complex, a T wave and a U wave which is rarely visible. Each of these waves appears as a result of the conduction signals of the heart.
P waveThe P wave represents the atrial depolarization; the signal that spreads from the SA node throughout the atria until the waves reaches the AV node. The time duration for the P wave is usually 0.08 to 0.1 seconds, and the amplitude is around 0.25 mV.
The period of zero voltage immediately after the P wave represents the time in which the impulse travels within the AV node. The atrial rate is calculated by determining the time interval between the P waves. An important parameter related to the P wave is the PR interval. This is the time period from the onset of the P wave to the beginning of the QRS complex. It normally ranges between 0.12 and 0.20 seconds in duration. It represents the time interval between the atrial depolarization and the onset of the ventricular depolarization. AV blocks and first-degree heart blocks can be diagnosed using the values of the PR interval.
QRS complexThe QRS complex represents ventricular depolarization, the passage of the signals from the AV node to the ventricles through the Bundle of His and Purkinje fibers. The normal duration of the QRS complex is 0.06 to 0.1 seconds. They have amplitude of 1.60 mV, which is much larger than the P wave. Determining the time interval between QRS complexes can help calculate the ventricular rate. Bundle branch blocks can be diagnosed easily by calculating the QRS intervals. The time interval from the beginning of the T wave is called the absolute refractory period, in which no conduction takes place, and the cells get ready for the next stimulation.
T waveThe T wave represents the recovery period of the heart muscles from the ventricular stimulations. It has amplitude of 0.1 to 0.5 mV. The relative refractive period refers to the last half of the T wave. The abnormalities of the ST segment are often an indication of the Ischemic heart, which is a condition in which the heart does not get enough oxygen, with blockage in the artery being the usual reason.
U waveU wave is a wave in ECG that is normally invisible. It is thought to be caused by repolarization of Purkinje fibers. Abnormalities in the U wave can help diagnose conditions such as hypercalcemia, thyrotoxicosis and hypokalemia. Myocardial ischemia can be identified from the appearance of an inverted U wave.
Disorders and Treatments
Learning objectives:
- Understand how blood lipids are implicated in cardiovascular diseases.
- Learn about common cardiovascular disorders and treatment options.
Important terminology:
a. Blood Lipids
Blood lipids are found either free or bound to other molecules. Blood lipids are composed of: cholesterol, high density lipoprotein, low density lipoprotein, very low density lipoprotein, free fatty acid, chylomicrons, and triglycerides.
b. Cholesterol
The word cholesterol comes from a Greek word (chole – bile; stereos – solid). It is a waxy steroid metabolite present in the cell membranes and lipoproteins of humans, as well as animals. It is transported in blood plasma.
The following media (Cholesterol) explains about the Cholesterol:
C. LipoproteinThe molecular complexes that consist of lipids and proteins are called lipoproteins. It is a typical example for conjugated proteins. They serve as transport vehicles for lipids such as cholesterol, triacylglycerol etc. in blood plasma and deliver them to various tissues for utilization.
d. TriacylglycerolAn ester compound composed of a glycerol bound to three fatty acids. Vegetable oil and animal oil are the major source of triacylglycerol.
Lipids Levels:
Cholesterol chart for adults
| Total cholesterol | HDL cholesterol | |
| Good | Less than 200 (but the lower the better) | Ideal is 60 or higher; 40 or higher for men and 50 or higher for women is acceptable |
| Borderline to | Moderately elevated | 200-239 |
| 150-199 | High | 240 or higher |
| 200 or higher; 500 considered very high | Low | n/a |